Interview with Dr. Iuliano about her study on the effect of higher dairy consumption (according to the recommendations) on reducing the risk of bone and hip fractures in the elderly. A plea for adapting the food supply in elderly care.
Interview with Dr. Iuliano about her study on the effect of higher dairy consumption (according to the recommendations) on reducing the risk of bone and hip fractures in the elderly. A plea for adapting the food supply in elderly care.
By dr. Stephan Peters (Dutch Dairy Association)
What are the main results of your study?
Older adults living in care facilities in Australia consume, on average, about 2 servings of dairy per day. When we increased that intake to 3.5 servings – the recommended amounts – we saw a relative risk reduction of 33% for all types of fractures, of 46% for hip fractures and of 11% for falls. We saw no change in the number of deaths. This is scientific evidence that the consumption of foods high in calcium and protein (such as milk, yogurt, cheese) in the recommended amounts reduces the risk of bone fractures in older adults compared to an intake below the recommended amounts. Australian guidelines recommend a daily intake of 4 servings of dairy for older women and 3.5 servings for older men, so our results are in line with that. A serving in Australia is 250 ml of milk, 40 g of cheese, and 200 g of yogurt.
How do you explain these results?
The results show that the consumption of dairy products in the recommended amounts is related to slowing the decline in volumetric bone mineral density: no significant loss was apparent after 12 months. In older adults who consumed fewer dairy products, we did see a loss in volumetric bone mineral density. Also, the muscles in the arms and legs of the dairy group remained stable, while muscle loss occurred in the control group. These differences may explain the beneficial effects we observed because they go beyond the effects of the nutrients in dairy on bone health. We saw that muscle mass and strength were preserved, and this too may account for the reduction in fractures and falls in the older adults in the dairy group.
Why did you conduct this study? Dairy is known to protect against fractures, right?
The link between dairy intake and fractures was actually an assumption until now. Based on intervention studies, it was assumed that dairy intake has a beneficial effect on bone growth and mineralization and on reducing bone decline. But results for fractures were extrapolated from observational and exploratory studies that described only correlations. The necessary evidence based on a properly conducted, randomized clinical trial that confirmed these assumptions had never been provided until our study.
What was your role in the study?
I was the principal investigator; I designed and led the study. I took care of all the care settings and participants and maintained contact with the management of the care settings. I was not involved in testing or analyses, because I would have known which groups the different institutions were assigned to and I needed to stay in touch with facility management.
What did you learn and experience while conducting this study?
What surprised me the most was that by simply improving the quality of nutrition we can make such a big difference to the lives and health of older adults in aged care. I now have in my hands the evidence with which to advocate for changes in food provision in aged care. And I have already presented the evidence to the “Royal Commission into Aged Care” who are investigating this on behalf of the government. This study has given me a voice and I can now influence change in a positive direction.
Which organizations funded the study and did that affect the outcome?
The study was conducted by the University of Melbourne and was partly funded by dairy organizations. The funders had no say in the design and execution of the study, nor in the publication of the results. I am very grateful for the funding from the industry, because without that support the project would not have been carried out. We would not have been able to demonstrate the importance of good nutrition for the health of older adults.
You could also have included an alternative plant-based group in your study. Why did you not do so? And would you have expected the same results?
There are a couple of reasons for this. First, an additional group would have doubled the cost of the study. In addition, older adults do not have the ability to consume the amount of plant-based calcium sources that would be required to have sufficient calcium. The average older adult in our study consumed less than 2 kg of food per day. In order to get the recommended amount of calcium they would have to consume 4 kg of plant-based calcium sources! We asked the residents what they wanted to eat and paid attention to their preferences. Many of the older adults had grown up with foods such as dairy products. Therefore, we offered them products that they already liked to eat.
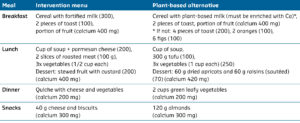
Can you provide an example of a 2 kg daily diet with dairy from your study, and a 4 kg daily diet with plant-based alternatives that contains the same amount of calcium?
Yes, of course. Below are two examples of daily foods that meet the recommendations for calcium. The intervention menu is with dairy and next to it is the fully plant-based alternative.